This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Hysteroscopy Special Interest Group (SIG) led by Chair, Erica Robinson, MD.
Access to SurgeryU and JMIG are two of the many benefits included in AAGL membership. The SurgeryU library features high-definition surgical videos by experts from around the world. JMIG presents cutting-edge, peer-reviewed research, clinical opinions, and case report articles by the brightest minds in gynecologic surgery.
SurgeryU video recommendations by our SIGs are available for public access for a limited time. The links to JMIG article recommendations are accessible by AAGL members only. For full access to SurgeryU, JMIG, CME programming, and member-only discounts on meetings, join AAGL today!
NEW to SurgeryU:
Isthmocele with Myometrial Cysts Hysteroscopy Repair
by Jovana Tavcar MD, FACOG
This video shows surgical technique for hysteroscopic resection of cesarean section scar defect, with additional challenge posed by myometrial cysts adjacent to the isthmocele, in a patient with persistent fluid in the cavity and multiple failed embryo transfers.
Jovana Tavcar MD, FACOG

Dr. Tavcar is a member of the AAGL Hysteroscopy SIG and Assistant Professor at Medstar Georgetown University Hospital in Washington, D.C.
SIG Recommended Video #2:
Hysteroscopic Resection of FIGO Type 3 Fibroids – The Uterine Deflation Technique
by Liron Bar-El, MD and Linda Bradley, MD
This is an excellent description of the complex surgical techniques and ultrasound guidance needed for the challenging resection of a Type 3 fibroid.
SIG Recommended Video #3:
Visual D&C for a 5 Weeks Missed Abortion
by Sergio Haimovich, MD
This is an unedited 2-minute video demonstrating the cold looping techniques using the resectoscope for surgical management of a 5-week missed abortion. This technique avoids the risk of intrauterine adhesions caused when performing a blind D&C.
JMIG Article Recommendation #1:
AAGL Practice Report: Practice Guidelines on Intrauterine Adhesions Developed in Collaboration With the European Society of Gynaecological Endoscopy (ESGE)
This publication is special due to the collaboration between the two largest Gynecology Endoscopy societies, the European ESGE, and the AAGL.
It is a complete guideline on intrauterine adhesions. Clarifies the definition, diagnosis, classification, prevention (both primary and secondary) but most important the management. It is a very recommended reading.
JMIG Article Recommendation #2:
Uterine Septum and Other Müllerian Anomalies in a Recurrent Pregnancy Loss Population: Impact on Reproductive Outcomes
by Bahi Fayek, MBBCh, MD, MSc, Emily C. Yang, BSc, MD, Yang (Doris) Liu, MSc, Vanessa Bacal, MD, MSc, FRCSC, Faten F. AbdelHafez, MD, MSc, PhD, and Mohamed A. Bedaiwy, MD, PhD, FACOG, FRCSC
Uterine septum has become a controversial topic. Is there any benefit of the removal for the perinatal outcome or not? This retrospective cohort study with a high never of patients, 377, brings more light to the importance of the septoplasty. Patients with septate uterus who received hysteroscopic septum division had a higher tendency to achieve more live births than those who elected expectant management.

Futurism and Hysteroscopy
For many years, bipolar resection was the most prominent method of intrauterine surgery. More recent years have seen the emergence of exciting new transcervical technologies.
Hysteroscopic morcellators are the “new kid on the block,” allowing removal of polyps, fibroids, and other intrauterine pathology without using electrical energy. Additionally, resected tissue is removed through the outflow system and caught in traps, eliminating the difficulty with “chip removal.” This can sometimes make hemostasis and visualization more difficult, and surgeons may lose a bit of “fine touch dissection” possible with cold loops. The advantages have propagated the system into wide use.
Some advances have come not from fundamental changes to surgical techniques, but from streamlined and easier to use technological systems. Mini-resectoscopes (1) and disposable hysteroscopes, such as CooperSurgical’s Endosee and the LiNA Medical Operascope have allowed office hysteroscopy to become more widely accessible.
Other new transcervical techniques include the Sonata system, a transcervical fibroid ultrasound identification and radiofrequency ablation system. Early data from a 3-year trial of the device suggests a decrease in fibroid symptoms on validated symptom scales for women treated as well as high subjective satisfaction (2).
Another advance coming down the pike is the advent of robotic hysteroscopy. In this system, concentric tube robots are passed through an endoscopic sheath which allows two-handed traction and counter traction of tissue. Figure 1. The surgeon stands at a distance and controls the tube robots through an input device, improving the ergonomic experience. To date, this has been demonstrated in animal models of Asherman’s syndrome, polypectomy, myomectomy, and removal of embedded IUDs (3).
 Figure 1: Concentric tube robots, outer diameter 1.5mm using two-handed techniques to resect simulated endometrial polyp with an electrosurgical probe.
Figure 1: Concentric tube robots, outer diameter 1.5mm using two-handed techniques to resect simulated endometrial polyp with an electrosurgical probe.
What ideas exist that may translate into new hysteroscopic techniques or technology in the future? Some authors have suggested methods to sample the microbiota of the Fallopian tube for fertility evaluations (4). Other authors have used artificial intelligence to improve MRI description of the location of myomas and this resulted in improved hysteroscopic outcomes. The authors even suggest AI assisted MRI data could be used to build 3-D printed models of uteri and myomas preoperatively to minimize error in preoperatively locating myomas and educate patients (5).
Soon, we may be using AI to assist in visual diagnosis of endometrial lesions. Another study found that a deep learning neural network model was slightly better at identifying endometrial lesions including hyperplasia and cancer than three experienced gynecologists (6).
We are living in the advent of a technological revolution that will likely fundamentally change the way we practice medicine over the next decades. While many new and exciting ideas are growing, there will also be years of validating and determining the most medically ideal and cost-effective ways to integrate them. As always, it will be up to the surgeon to decide which method is most suited to the pathology, the patient, and the practice.
References:
- Dealberti D, Riboni F, Cosma S, et al. Feasibility and acceptability of office-based polypectomy with a 16Fr mini-resectoscope: a multicenter clinical study. J Minim Invasive Gynecol. 2016;23:418–424
- Lukes A, Green MA. Three-Year Results of the SONATA Pivotal Trial of Transcervical Fibroid Ablation for Symptomatic Uterine Myomata. J Gynecol Surg. 2020 Oct 1;36(5):228-233. doi: 10.1089/gyn.2020.0021. Epub 2020 Oct 1. PMID: 33061253; PMCID: PMC7548023
- Harvey, L., Hendrick R., Dillon, N., Webster, S., Webster, R., Anderson, T. A Novel Robotic Endoscopic Device Used for Operative Hysteroscopy. J Minim Invasive Gynecol. Published: June 12, 2020. Nov-Dec;27(7):1631-1635. DOI: 10.1016/j.jmig.2020.06.009. PMID: 32540499
- Vitale SG, Carugno J, D’Alterio MN, Mikuš M, Patrizio P, Angioni S. A New Methodology to Assess Fallopian Tubes Microbiota and Its Impact on Female Fertility. Diagnostics. 2022; 12(6):1375. https://doi.org/10.3390/diagnostics12061375.
- Chen M, Kong W, Li B, Tian Z, Yin C, Zhang M, Pan H, Bai W. Revolutionizing hysteroscopy outcomes: AI-powered uterine myoma diagnosis algorithm shortens operation time and reduces blood loss. Front Oncol. 2023 Dec 8;13:1325179. doi: 10.3389/fonc.2023.1325179. PMID: 38144535; PMCID: PMC10739391).
- Zhang, Y., Wang, Z., Zhang, J. et al.Deep learning model for classifying endometrial lesions. J Transl Med 19, 10 (2021). https://doi.org/10.1186/s12967-020-02660-x
About the Author:
Lara Harvey, MD, MPH

Dr. Harvey is a member of the AAGL Hysteroscopy SIG and Assistant Professor of OBGYN and FMIGS Program Director at Vanderbilt University Medical Center in Nashville, Tennessee.

Challenges Faced During Hysteroscopic Myomectomy Using a Hysteroscopic Tissue Removal System
Hysteroscopic tissue removal systems (HTRS) are game changers in treating intrauterine pathologies. Due to their high safety profile, effectiveness, shorter operative time and short learning curve, they are replacing the traditional resectoscopes (1). HTRS contribute to one-third of the U.S. market value (2). Though its efficacy is proven in polyps and placental remnants, its use in myomas, septum, and intrauterine adhesions comes with challenges.
Submucous myomas (SM) account for 15-20% of fibroids and are made of myometrial cells present in the endometrial cavity. They can cause abnormal uterine bleeding, infertility, or recurrent pregnancy loss. Hysteroscopic myomectomy (HM) is the procedure of choice for SM. They can be performed in-office or in the operating theatre. Different techniques are available such as the slicing method using electrosurgical current with a resectoscope, enucleation using mechanical instruments, electrode needle or laser, and HTRS.
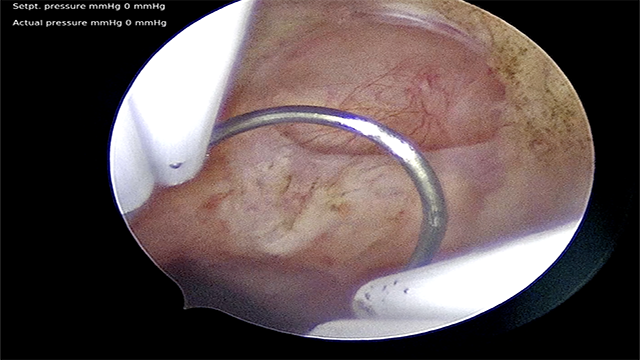
Going back to the basic formula of volume being a function of diameter, ν = πd3/6(3). Hence, as the size of the myoma increases, the volume triples. The HTRS works on the principle of cutting and aspiration. The success of the HM procedure will depend on the rate at which the myoma is resected, the fluid deficit and the procedure time. These in turn depend on the size, volume, consistency, location and type of myoma. Though HTRS works fine for myomas of soft consistency, type 0 to 1, (Image.1) and of size < 3 cm, it comes at a huge cost when compared to other techniques which are a lot cheaper.
The amount of tissue resected per minute during HM depends on (4):
- The contact between the cutting window and the pathology. (2,3.) (Image. 4.)
- The speed of cutting and suction
The difficulty arises in type 2 SM dense and calcified myoma, and there is a higher chance of shifting to a resectoscope (5). The technique of enucleation using HTRS has been tried for type 2 myomas, though there is no evidence to support this technique, it also poses a challenge of expertise, as there is a risk of uterine perforation as we go deeper in the muscle.
HTRS are mechanical and cannot coagulate the open vessels in case of excess bleeding, necessitating a second procedure.
A systemic review and meta-analysis to evaluate the HTRS in intrauterine pathologies, compared three systems – Truclear®, Myosure® or IBS® (Intrauterine Bigatti Shaver) with conventional resectoscope in 498 patients from 2010 to 2019. They did not find any difference in the operative time for complete removal of myoma between HTRS and conventional resectoscope. There was a significantly higher fluid deficit with HTRS compared to conventional resectoscopes (95% CI: 41.42 to 276.54; P=0.008), though none reported fluid overload (6).
All instruments come with their challenges. To achieve completion of the procedure with minimal or no complications requires the following:
- A good preoperative evaluation,
- the right selection of case,
- the right selection of the instrument,
- the availability of the instruments,
- Hospital or office setup, institutional or private
- the surgeon’s expertise
- Insurance coverage.
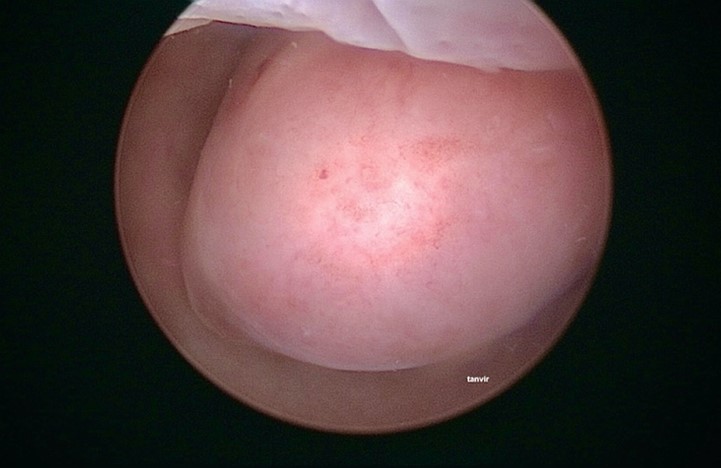 Image 1. Type 1 Submucous fibroid of 2.5 cm at the fundus
Image 1. Type 1 Submucous fibroid of 2.5 cm at the fundus

Image 2: In-office myomectomy using Hysteroscopic tissue removal system with a rotatory blade.

Image 3: In-office myomectomy using Hysteroscopic tissue removal system with a rotatory blade.
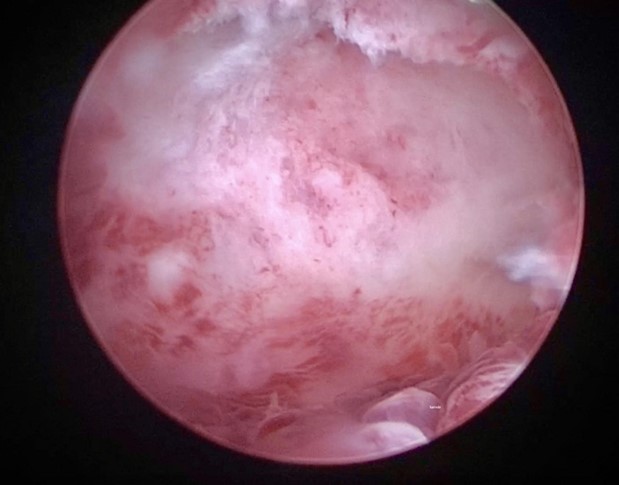
Image 4: Panoramic view following in-office myomectomy.
REFERENCES
- Franchini, M., et al (2021) Mechanical hysteroscopic tissue removal or hysteroscopic morcellator: understanding the past to predict the future. A narrative review, Facts Views Vis Obgyn, 13 (3): 193-201
- Ren, F, et al (2022) Comparison of Hysteroscopic Morcellation Versus Resectoscopy in Treatment of Patients with Endometrial Lesions: A Meta-Analysis, Medical Science Monitor,
- Greenberg JA, Adam R, Chin A, Sullivan R. Ex-vivo myoma morcellation. Interlace Medical, Inc.; 2008.
- Cohen S, Greenberg JA. Hysteroscopic morcellation for treating intrauterine pathology. Rev Obstet Gynecol. 2011 Summer;4(2):73-80. PMID: 22102930; PMCID: PMC3222940.
- Van Wessel S., van Vliet H., Schoot B.C., Weyers S., Hamerlynck T.W. Hysteroscopic morcellation versus bipolar resection for removal of type 0 and 1 submucous myomas: A randomized trial. EJOG. 2021;259:32–37.
- Yin X, Cheng J, Ansari SH, Campo R, Di W, Li W, Bigatti G. Hysteroscopic tissue removal systems for the treatment of intrauterine pathology: a systematic review and meta-analysis. Facts Views Vis Obgyn. 2018 Dec;10(4):207-213.
About the Authors:
Alka Kumar, MBBS, MS Tanvir Singh, MBBS, MS


Dr. Kumar is a member of the AAGL Hysteroscopy SIG, Director of the Women’s Health Centre in Jaipur, India and Consultant Advisor at Max Society of Medical Academics, Innovation and Research in Saket, New Delhi, India.
Dr. Tanvir Singh is an ObGyn and Consultant at Tanvir Hospital in Hyderabad, India.

Claiming Confrontations in Hysteroscopic Septoplasty
Septate uterus is the most common Müllerian anomaly in women with an estimated incidence of 0.2–2.3%, subject to the diagnostic methods and classification system.1 It can be categorized into partial (sub-septate) or complete septate groups and is accountable for poor reproductive outcomes and obstetric problems, such as pregnancy loss, preterm birth and fetal malpresentations.2 The most commonly seen reproductive complication is spontaneous miscarriage, affecting more than 60% of women with uterine septum. It has been proposed that abnormal implantation dynamics caused by poor blood supply to the septum leads to spontaneous miscarriages.3
Hysteroscopic Septal Resection- A blanket therapy?
Surgical correction through hysteroscopic septum resection is the preferred treatment for symptomatic septate uterus, particularly in cases of recurrent miscarriages, infertility, or significant uterine anomalies. The role of uterine septum in adverse pregnancy outcomes and the indications for uterine septum resection remains controversial.4
Resection of uterine septum provides a multifaceted approach to improving reproductive health. By correcting uterine anomalies, it optimizes the uterine environment, enhancing the chances of successful implantation and pregnancy. This procedure also mitigates obstetric risks such as intrauterine growth restriction, malpresentation, and preterm labor, thereby promoting safer pregnancies. Additionally, by eliminating the physical barrier hindering embryo implantation, resection fosters improved trophoblastic invasion, ultimately enhancing the establishment of a pregnancy.5 The benefits extend to assisted reproductive techniques, where optimizing the uterine cavity for embryo transfer and implantation leads to augmented success rates. Furthermore, resection promotes menstrual regularity by alleviating obstructive effects on menstrual flow, aiding in ovulatory synchronization and fertility optimization. By relieving anatomical constraints and optimizing endometrial receptivity through improved vascularity, glandular function, and cytokine milieu, resection facilitates a conducive environment for embryo implantation. Beyond the physical benefits, successful resection also offers psychological reassurance, fostering emotional well-being and resilience throughout the reproductive journey.
Although it is a relatively expeditious, efficient and safe method, it can also be associated with complications that may adversely affect reproductive performance.
Uterine septum resection carries several potential risks and complications. These include iatrogenic endometrial injury, which can impair endometrial receptivity and implantation potential, and the possibility of developing Asherman’s syndrome, characterized by intrauterine adhesions and menstrual abnormalities.6 Surgical intervention may also disrupt uterine vasculature, leading to compromised blood flow and impaired embryo implantation. Furthermore, manipulation of the uterine cavity can disrupt myometrial integrity and contractile function, potentially resulting in dysfunctional labor patterns.7 There’s a risk of uterine wall weakness and dehiscence, particularly during pregnancy or labor, necessitating emergency obstetric interventions. Additionally, surgical trauma induces an inflammatory response in the uterine microenvironment, potentially impacting cytokine profiles and immune cell dynamics, which could adversely affect implantation and pregnancy maintenance.8
Hysteroscopic septoplasty stands as a highly effective and minimally invasive intervention for correcting uterine septa and associated reproductive morbidities. Supported by robust clinical evidence, hysteroscopic septoplasty stands resolute as the quintessential cornerstone in the armamentarium of gynecological surgical interventions, delineating a paradigm shift towards enhanced reproductive health outcomes and bolstered patient satisfaction within the realm of uterine corrective procedures.
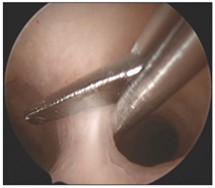 Image 1: Septal resection using cold scissors.
Image 1: Septal resection using cold scissors.
 Image 2: Septal resection using Bipolar Resectoscope.
Image 2: Septal resection using Bipolar Resectoscope.
REFERENCES
- Blanco-Breindel MF, Kahn J, Singh M. Septate Uterus. 2023 Jul 15. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 37603639.
- Pfeifer SM, Attaran M, Goldstein J, Lindheim SR, Petrozza JC, Rackow BW, Siegelman E, Troiano R, Winter T, Zuckerman A, Ramaiah SD. ASRM müllerian anomalies classification 2021. Fertil Steril. 2021 Nov;116(5):1238-1252
- Jacquinet A, Millar D, Lehman A. Etiologies of uterine malformations. Am J Med Genet A. 2016 Aug;170(8):2141-72
- Nouri K, Ott J, Huber JC, Fischer EM, Stögbauer L, Tempfer CB. Reproductive outcome after hysteroscopic septoplasty in patients with septate uterus: a retrospective cohort study and systematic review of the literature. Reprod Biol Endocrinol. 2020;8:52
- Bosteels J, Weyers S, Puttemans P, et al. The effectiveness of hysteroscopy in improving pregnancy rates in subfertile women without other gynaecological symptoms: a systematic review. Hum Reprod Update. 2010;16:1–11
- Kowalik CR, Goddijn M, Emanuel MH, Bongers MY, Spinder T, de Kruif JH, Mol BW, Heineman MJ. Metroplasty versus expectant management for women with recurrent miscarriage and a septate uterus. Cochrane Database Syst Rev. 2011 Jun 15;(6):CD008576. doi: 10.1002/14651858.CD008576.pub3. Update in: Cochrane Database Syst Rev. 2017 Jan 17;1:CD008576. PMID: 21678380.
- Rikken JF, Kowalik CR, Emanuel MH, Mol BW, Van der Veen F, van Wely M, Goddijn M. Septum resection for women of reproductive age with a septate uterus. Cochrane Database Syst Rev. 2017 Jan 17;1(1):CD008576. doi: 10.1002/14651858.CD008576.pub4. PMID: 28093720; PMCID: PMC6464821.
- Ahmed M. Abbas, Mohamed Abdallah, Armia Michael, Recurrent rupture uterus after hysteroscopic resection of uterine septum: A case report, Middle East Fertility Society Journal, Volume 22, Issue 4,2017(340-342) ISSN 1110-5690, https://doi.org/10.1016/j.mefs.2017.02.002.
About the Authors:
Alka Kumar, MBBS, MS Vidya V. Bhat, MBBS, MD, DNB


Dr. Kumar is a member of the AAGL Hysteroscopy SIG, Director of the Women’s Health Centre in Jaipur, India and Consultant Advisor at Max Society of Medical Academics, Innovation and Research in Saket, New Delhi, India.
Dr. Bhat is a Hysteroscopy & Laparoscopic Surgeon, IVF Specialist and Medical Director at Radhakrishna Multispecialty Hospital & IVF Center in Bengaluru, India.
The post Spotlight On: Hysteroscopy appeared first on NewsScope.