This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Pelvic Pain Special Interest Group (SIG) led by Chair, Susan Khalil, MD.
Access to SurgeryU and JMIG are two of the many benefits included in AAGL membership. The SurgeryU library features high-definition surgical videos by experts from around the world. JMIG presents cutting-edge, peer-reviewed research, clinical opinions, and case report articles by the brightest minds in gynecologic surgery.
SurgeryU video recommendations by our SIGs are available for public access for a limited time. The links to JMIG article recommendations are accessible by AAGL members only. For full access to SurgeryU, JMIG, CME programming, and member-only discounts on meetings, join AAGL today!
SIG Recommended SurgeryU Video #1:
Chronic Pelvic Pain: A Guide to Perform a Focused Physical Exam
Christana O Ajewole, MD, Dorothy Bestoyong, DO, Chensi Ouyang, MD, Jessica Brooke Feranec, MD, Georgine Lamvu, MD, and Jorge F. Carrillo, MD
This outstanding video demonstrates a comprehensive approach to the workup, clinical evaluation, and focused physical exam in patients experiencing pelvic pain. One of the key aspects of pelvic pain management is identification of pain generators and triggers, and learning the steps to perform a thorough clinical assessment is extremely valuable. This video received the IRCAD award at the 2022 AAGL Global Congress.
SIG Recommended SurgeryU Video #2:
Pelvic Nerves in Laparoscopy: A Review of Anatomy and Approach to Dissection
Shabnam Gupta, MD and Jon I. Einarsson, MD
Neuropelveology is an emerging topic in minimally invasive surgery but can be challenging to learn. This video demonstrates many important nerves that can be encountered during laparoscopic surgery and highlights important anatomic considerations. An understanding of the nerves in the pelvis are critical for preserving function, avoiding injury, and identifying pathology that may involve these structures.
JMIG Article Recommendation #1:
Developing a Predictive Model for Minimal or Mild Endometriosis as a Clinical Screening Tool in Infertile Women: Uterosacral Tenderness as a Key Predictor
Jie Zhang, MM, Jing Wang, MD, PhD, Jingyi Zhang, MM, JinLiu, PhD, Yanhong Xu, MM, Peipei Zhu, MM, Lei Dai, MM, Li Shu, MD, PhD, Jinyong Liu, MD, PhD, Zhen Hou, MD, PhD, Feiyang Diao, MD, Jiayin Liu, MD, PhD, and Yundong Mao, MD, PhD
Endometriosis can be challenging to diagnose in patients with pelvic pain, and imaging modalities lack sensitivity in ruling in disease. This study aims to develop a non-invasive physical exam assessment to screen individuals with pelvic pain for endometriosis based on a compilation of cost-effective tools.
JMIG Article Recommendation #2:
Identifying Gaps in Pelvic Pain Education: A scoping Review and Structured Analysis of Obstetrics and Gynecology Training Milestones
Mario E. Castellanos, MD, Jorge F. Carrillo, MD, Isabel Green, MD, MHPE, Alexandra Milspaw, PhD, Med, and Georgine Lamvu, MD, MPH
Pelvic pain is a challenging diagnosis due to highly variable symptoms, severity, and a broad differential diagnosis. Furthermore, educational curriculum on pelvic pain assessment and treatment is lacking. This scoping review aimed to identify gaps and areas for improvement in pelvic pain education.

Emerging Trends in Neuropelveology
Neuropelveology is an emerging clinical discipline aimed at understanding the concept of the pelvic nervous system and its specific pathology. It requires a cross-disciplinary approach as there is currently no clinical discipline that can manage all aspects. The concept was introduced twenty years ago by Possover with increasing awareness in the gynecologic surgery field1.
Neuropelveology goals are to increase safety and improve surgical outcomes through nerve sparring surgical techniques, to represent the foundation of treatment of intrapelvic neuropathies and chronic pelvic pain, and to restore function2.
Learning pelvic neuroanatomy is imperative for pelvic surgeons to make an appropriate diagnosis and avoid complications. As such, there is tremendous interest in gynecology to learn about neuroanatomy. A collaborative approach on the teaching modalities under the guidance of experts and interested surgical societies will benefit generations of surgeons. As an emergent discipline, it will be helpful to establish a roadmap to success with measurable and meaningful outcomes3.
Interventional procedures for treatment of chronic pelvic pain should be done by appropriately trained surgeons. One classic example is the laparoscopic implantation of neuroprosthesis procedure (LION) in which electrodes are selectively placed in contact with the pelvic nerves. This offers the option of treatment of chronic pelvic pain through neuromodulation but has not been studied in a randomized control trial. Potential side effects and complications will require prospective evaluation4. Another application is pudendal nerve stimulation for the treatment of hyperactive bladder, urinary and fecal incontinence, and improved sexual function5.
The LION procedure could also be a treatment option for paraplegic patients by initiating improved motor function. To do this, somatic nerves such as sciatic, pudendal, and femoral are bilaterally stimulated with electrodes inserted transperitoneal through a laparoscopic approach. Continuous or variable stimulation, with currents frequency 5-60Hz and pulse width 50–150 µs, are employed based on the type of nerves stimulated and function goals6. Individuals suffering from spina bifida may be another group of patients who could benefit from this type of intervention. Observed data indicated an interesting result of increased leg lean mass and possible increase in bone mineral content. This has opened the concept of use in the therapeutics of osteoporosis, cardiovascular disease, or even as potential preventative care7.
While neuropelveology was introduced more than 20 years ago as an emerging discipline to deal with complex pelvic neurological questions, it is upon us to understand its role and advantages and how to incorporate it safely in the gynecological practice. There are already new trends for potential use of its interventional arm that bridges to other clinical domains and highlights the prime role of pelvic health clinicians and researchers8.
References
- Possover M, Forman A, Rabischong B, Lemos N, Chiantera V. Neuropelveology: New Groundbreaking Discipline in Medicine. J Minim Invasive Gynecol. 2015 Nov-Dec;22(7):1140-1. doi: 10.1016/j.jmig.2015.06.009. Epub 2015 Jun 20. PMID: 26099648.
- Lemos N, Possover M. Laparoscopic approach to intrapelvic nerve entrapments. J Hip Preserv Surg. 2015 Jul;2(2):92-8. doi: 10.1093/jhps/hnv030. Epub 2015 Jun 6. PMID: 27011825; PMCID: PMC4718483.
- Marcu I, Balica A, Gavard JA, Campian EC, Fernandes GL, Solnik MJ, Morozov V, Lemos N. Closing the knowledge gap in pelvic neuroanatomy: assessment of a cadaveric training program. BMC Med Educ. 2021 Jan 7;21(1):26. doi: 10.1186/s12909-020-02443-4. PMID: 33413351; PMCID: PMC7792346.
- Possover M, Baekelandt J, Chiantera V. The Laparoscopic Implantation of Neuroprothesis (LION) Procedure to Control Intractable Abdomino-Pelvic Neuralgia. Neuromodulation. 2007 Jan;10(1):18-23. doi: 10.1111/j.1525-1403.2007.00083.x. PMID: 22151808.
- Possover M. A novel implantation technique for pudendal nerve stimulation for treatment of overactive bladder and urgency incontinence. J Minim Invasive Gynecol. 2014 Sep-Oct;21(5):888-92. doi: 10.1016/j.jmig.2014.03.026. Epub 2014 Apr 18. PMID: 24747099.
- Løve US, Elmgreen SB, Forman A, et al. Surgical Aspects of the Possover LION Procedure: An Emerging Procedure for Recovery of Visceral Functions and Locomotion in Paraplegics. World J Lap Surg 2021;14(2):75–80
- Løve US, Kasch H, Severinsen KE, Abrahamsen J, Høyer C, Forman A, Thomsen HH. The Laparoscopic Implantation of Neuroprosthesis Procedure Increases Leg Lean Mass in Individuals With Paraplegia Due To Traumatic Spinal Cord Injury. Neuromodulation. 2023 Dec;26(8):1802-1807. doi: 10.1016/j.neurom.2022.04.044. Epub 2022 Jun 8. PMID: 35690509.
- Possover M. Neuropelveology: An Emerging Discipline for the Management of Pelvic Neuropathies and Bladder Dysfunctions through to Spinal Cord Injury, Anti-Ageing and the Mars Mission. J Clin Med. 2020 Oct 13;9(10):3285. doi: 10.3390/jcm9103285. PMID: 33066247; PMCID: PMC7656309.
About the Author:
Adrian Balica, MD

Dr. Balica is a member of the AAGL Pelvic Pain SIG, Vice Chair for Clinical Affairs and Clinical Professor at the Department of Obstetrics and Gynecology University of South Carolina/ Prisma Health in Columbia, South Carolina.

An Unusual Case of Pelvic Pain: Chronic Ovarian Torsion
Ovarian torsion is a well-known cause of acute pelvic pain, particularly in cases with a known adnexal mass causing instability of the utero-ovarian and infundibulopelvic ligaments. Ovarian torsion is characterized by a sudden onset of sharp abdominal pain and can be associated with nausea and vomiting. Pain often does not respond to acetaminophen or non-steroidal anti-inflammatory medications and many patients present to the emergency department due to severity of symptoms.
This is a case of a 22-year-old female who presented to the ambulatory clinic for a second opinion regarding a right adnexal mass. She was studying in the library and had severe pain in her right abdomen 3 months prior. She sought emergency care. A pelvic ultrasound revealed a 7.5cm right ovarian cyst, and she was discharged with instructions to follow up with a gynecologist. The severe pain improved but did not fully resolve, and she developed heaviness and discomfort in this region.
Pelvic magnetic resonance imaging (MRI) showed an edematous ovary with peripheralization of follicles, no discrete cyst, and twisted appearance of the ovarian vessels with concern for torsion. Given these findings, laparoscopic ovarian de-torsion was recommended, and the patient proceeded to the operating room the following day.
At the time of laparoscopy, the right adnexal structures were twisted around their pedicles twice. The ovary was significantly enlarged, but there was no evidence of necrosis or tissue damage (Figures 1A and 1B). Due to suspicion for chronic torsion and resulting edema of the ovary, oophoropexy was performed via plication of the utero-ovarian ligament and attachment to the ovarian stroma to minimize mobility of the enlarged ovary.
Figure 1: Laparoscopy showing right adnexal torsion before (1A) and after (1B) untwisting of the pedicle
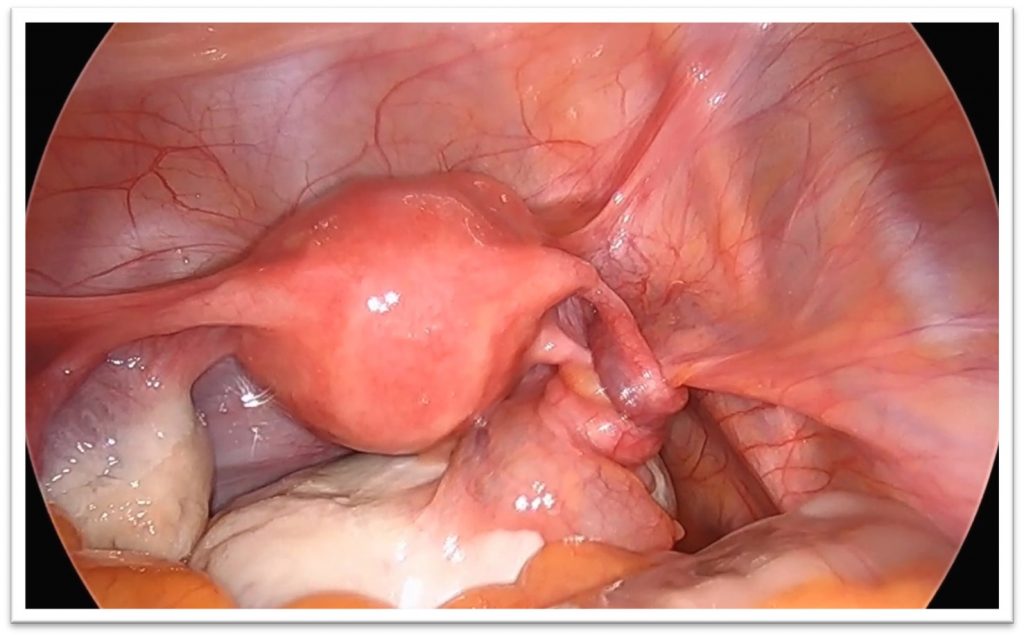 Figure 1A
Figure 1A
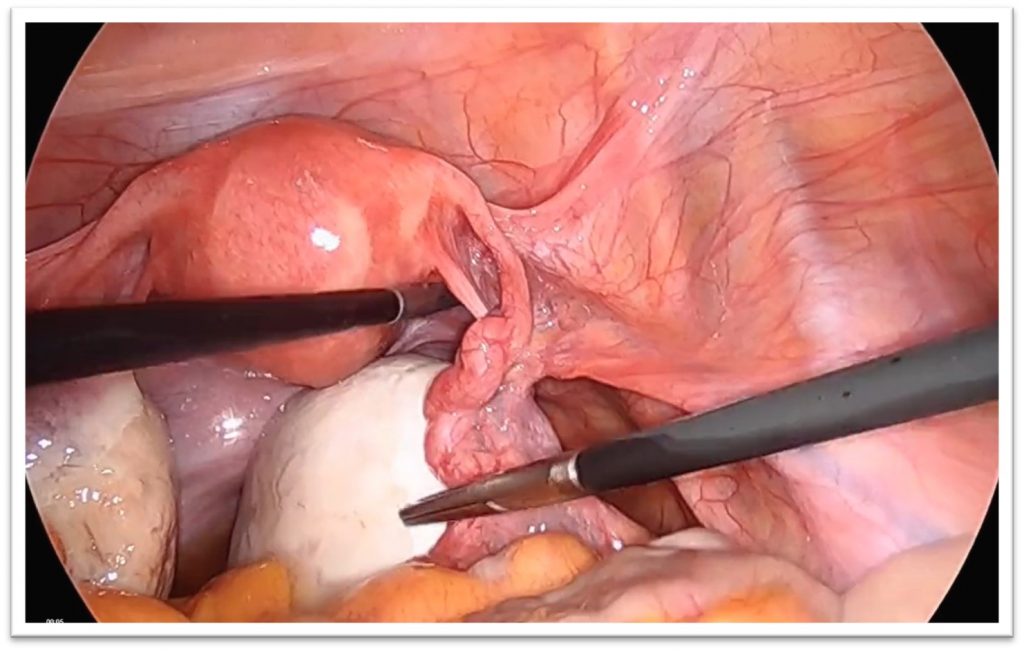 Figure 1B
Figure 1B
The patient did well post-operatively initially. Approximately 11 months later, she returned to the emergency department with excruciating right lower quadrant pain. The pain was very similar to her initial presentation of torsion, and was associated with nausea, vomiting, and lack of appetite. Pelvic ultrasound revealed an enlarged right ovary measuring 7cm with absent vascular flow. Diagnostic laparoscopy revealed acute torsion of the right adnexa with edema and ecchymosis (Figures 2A and 2B). Ovarian de-torsion and repeat oophoropexy was performed; this time, the ovary was secured to the round ligament with two sutures to help with stabilization.
Figure 2: Laparoscopy showing right ovarian torsion before (2A) and after (2B) untwisting of the pedicle
 Figure 2A
Figure 2A
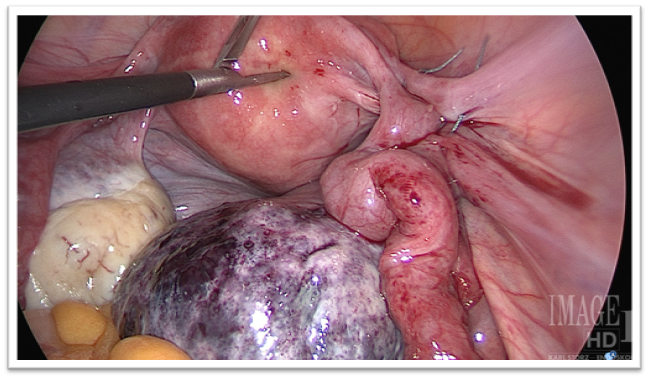 Figure 2B
Figure 2B
Five months later, the patient returned to the emergency department with recurrent pain. Pelvic ultrasound revealed a persistently enlarged right ovary with absent flow. Due to her third episode of recurrent torsion, the patient requested oophorectomy for definitive management. Laparoscopy revealed torsion despite presence of the prior oophoropexy sutures. She underwent an uncomplicated right salpingo-oophorectomy.
While ovarian torsion can re-occur, multiple recurrences in the setting of oophoropexy is rare. We suspect that this patient had chronic torsion during her initial episode which resulted in permanent enlargement and edema of the ovary. This likely destabilized the adnexal axis and pre-disposed her to abnormal movement of the vascular supply. This case is important to encourage providers to consider atypical presentations of acute pelvic pain and to have a high index of suspicion for ovarian torsion.
Figure 3: Laparoscopy showing right ovarian torsion before (3A) and after (3B) oophorectomy
 Figure 3A
Figure 3A
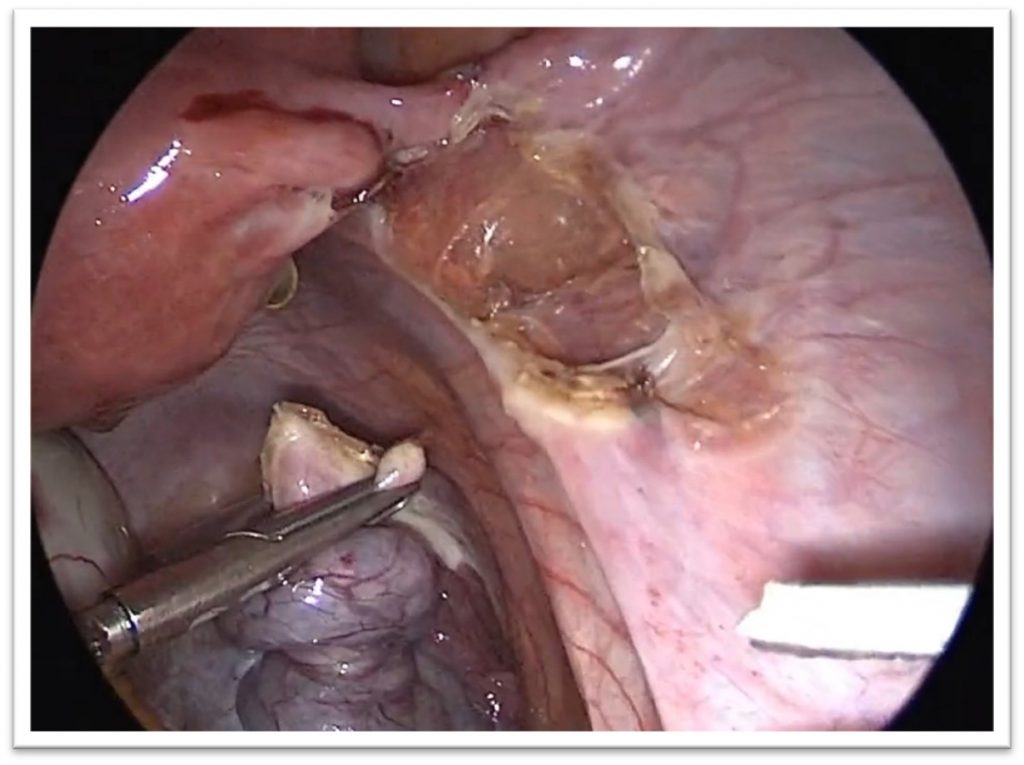 Figure 3B
Figure 3B
About the Author:
Aakriti R. Carrubba, MD

Dr. Carrubba is a member of the Pelvic Pain SIG and Assistant Professor of Obstetrics and Gynecology Consultant, Minimally Invasive Gynecologic Surgery, Medical and Surgical Gynecology at the Mayo Clinic in Jacksonville, Florida.
The post Spotlight On: Pelvic Pain appeared first on NewsScope.