
This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Urogynecology and Vaginal Surgery Special Interest Group (SIG) led by Chair, Lauren Siff, MD.
Access to SurgeryU is one of the many benefits included in AAGL membership. The SurgeryU library features high-definition surgical videos by experts from around the world.
SurgeryU video recommendations by our SIGs are available for public access for a limited time. For full access to SurgeryU, JMIG, CME programming, and member-only discounts on meetings, join AAGL today!
SIG Recommended SurgeryU Video #1:
A Stepwise Approach to Lefort Colpoleisis
By: Samantha Benlolo, MD, FRCSC, Elizabeth Miazga, MD, Annette Epp, MD, Alysha Nensi, MD, MSc, FRCSC, and Dana Soroka, MD, FRCSC
This is a high-quality video walking the viewer through one of our most successful yet infrequently performed transvaginal prolapse procedures. The video features nice picture in picture views correlating surgical footage and simulation so one could practice this outside of the operating room. This is useful as it can be challenging to wrap your head around this procedure with such distorted anatomy in the setting of advanced prolapse.
SIG Recommended SurgeryU Video #2:
Technique for Complicated Bladder Dissection: Bladder Transillumination with Firefly® Technology
By: Alexandra C.E. Dadrat, MD, Maria G. Duarte, MD, and Elisha McKay, MD
Check out this video showing a nice technique for those difficult bladder dissections. This robotic hysterectomy and sacrocolpopexy shows concurrent use of white light cystoscopy and FireFly imaging technology as an easy safe method to aid in demarcating bladder margins during these complex dissections.

Role of Fluorescence-Guided Surgery (FGS) using Indocyanine Green (ICG) for Ureteric Visualization during Complex Gynaecological Procedures
Ureteric injuries are a significant risk during gynaecological surgeries, especially in complex cases involving severe endometriosis, pelvic inflammatory disease, and gynaecologic cancers. The prevalence ranging from 0.5% to 10%1,2. Traditional methods for ureteral identification during surgery, such as cystoscopy-directed catheters and lighted ureteral stents3, have limitations in cost, application, and efficacy. Indocyanine Green (ICG) dye has emerged as a promising tool for enhancing the intraoperative visualization of the ureters.
ICG is a water-soluble fluorescent dye developed in the 1950s, fluoresces under near-infrared light, making it highly effective for real-time imaging of anatomical structures.
ICG is prepared by dissolving 25 mg in 10 ml of distilled water and further diluting 2 ml of this solution in 10 ml of distal water (concentration of 2.5 mg/ml). A 5F ureteral catheter guided over GLIDEWIRE® Hydrophilic Terumo guidewires is inserted into each ureter, and 5 ml of the diluted ICG is administered retrograde via cystoscopy (Fig. 1a, b). Visualization was enhanced using a camera system with NIR overlay mode, allowing simultaneous viewing of the laparoscopic image and fluorescent ureters.
 Fig. 1a: External view showing the insertion of ureteric catheters through the operating sheath of a hysteroscope.
Fig. 1a: External view showing the insertion of ureteric catheters through the operating sheath of a hysteroscope.
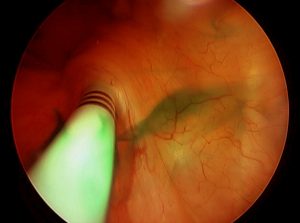 Fig. 1b: Cystoscopic view of ureteric catheter and ICG injection.
Fig. 1b: Cystoscopic view of ureteric catheter and ICG injection.
Over a 6-year period at our centre, we retrospectively reviewed the effectiveness of ICG in nearly 500 cases for ureter visualization during complex gynaecological surgeries. The study included patients undergoing procedures where ureteral identification was critical, such as endometriosis surgeries, both primary and repeat surgeries, (Fig. 2a, b) TLH with adhesions, and other complex cases like post-hysterectomy cysts, retroperitoneal masses, frozen pelvis due to infectious pathologies, and large cervical and broad ligament myomas.
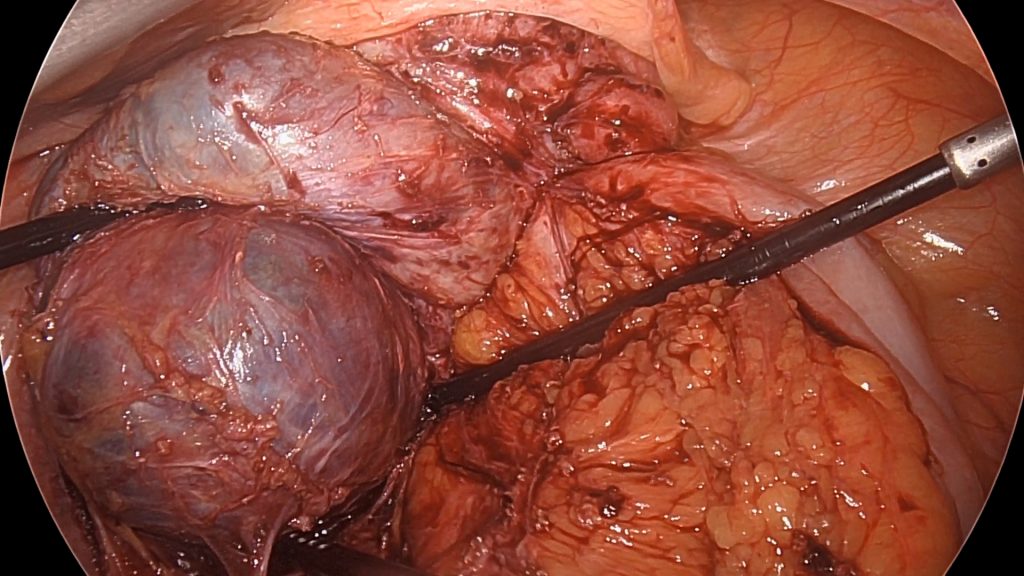 Fig. 2a: Initial intraoperative view during a third repeat surgery for severe endometriosis, including a large endometriotic cyst and deep infiltrative endometriosis (DIE).
Fig. 2a: Initial intraoperative view during a third repeat surgery for severe endometriosis, including a large endometriotic cyst and deep infiltrative endometriosis (DIE).
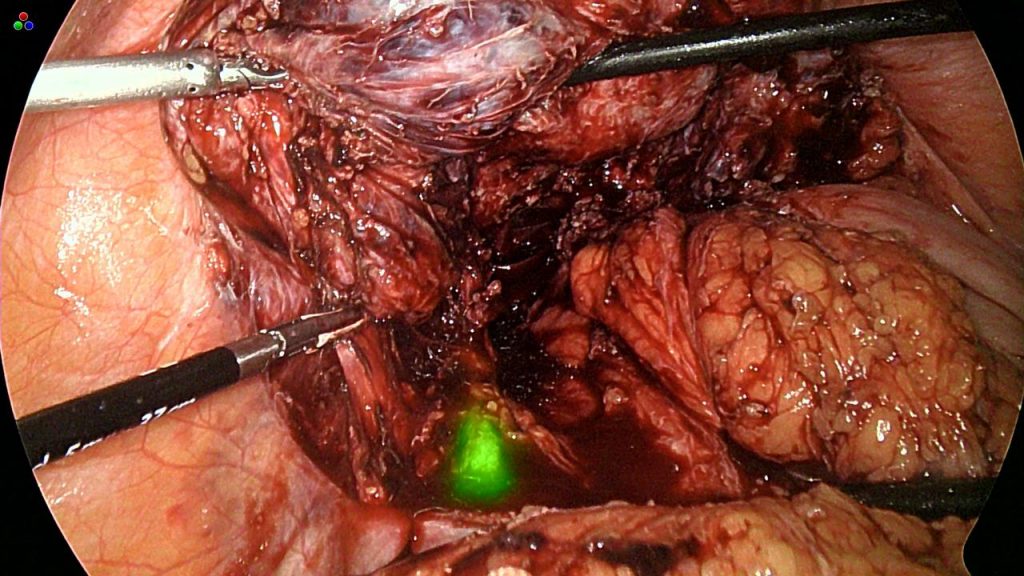 Fig. 2b: Clear visualization of the ICG-tagged ureter, facilitating further dissection.
Fig. 2b: Clear visualization of the ICG-tagged ureter, facilitating further dissection.
In our study, ureteral visualization was successful in all cases with complete ureteral visibility showing instantly without any time lag and staying as long as the duration of the surgery. We have noted ICG fluorescence up to five hours remains as bright as the first appearance from the pelvic brim up to the ureteric tunnel, making it a useful adjunct in challenging situations.
Our key finding was the effectiveness of ICG in preventing ureteral injuries. However, despite the use of ICG, two cases of ureteral thermal injury occurred during surgery for severe parametrial endometriosis. On recognizing, stenting was performed, and the patient’s recovery was uneventful. This incident underscores that while ICG significantly enhances visualization, this should not lead to a false sense of security, and all standard precautions must still be observed during surgery.
In our experience, FGS may become an indispensable part of complex gynecological procedures (Fig. 3), enhancing both the safety and efficiency of surgeries.
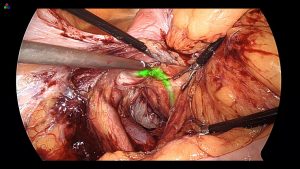
Fig. 3: Identification of an unusually medially displaced ureter made easier by ICG tagging.
For the novice, it can make their journey of foray into retroperitonium easier, and for expert endoscopists it provides safer navigation in extremes of anatomical distortions. In short, I would like to say we do not have to look up for the ureters, rather they show up on their own in the maze of adhesions. There are several other uses of ICG for sentinel node sampling in oncology, assessing bowel perfusion after resection anastomosis and in general surgery for gall bladder visualization. With widespread applications of FGS, the future camera systems will be equipped with ICG mode, making way for more universal application of ICG in gynaecological surgery.
References
- Liapis A, Bakas P, Giannopoulos V, Creatsas G. Ureteral injuries during gynecological surgery. *Int Urogynecol J Pelvic Floor Dysfunct.* 2001;12(5):391-393; discussion 394. https://doi.org/10.1007/PL00004045.
- Saidi M, Kentsadler R, Vancaillie T, et al. Diagnosis and management of serious urinary complications after major operative laparoscopy. *Obstet Gynecol.* 1996;87(2):272-276. PMID: 8598941.
- Linder B.J., Burnett T.L., Gebhart J.B. Lighted Ureteral Stent Placement for Challenging Endoscopic Gynecologic Surgeries. Abstract, Volume 25, Issue 7, Supplement, S241, November 2018. DOI: 1016/j.jmig.2018.09.624.
About the Authors
Nutan Jain, MS (Obstetrics and Gynecology)
Priyanka Sureddi, MS, DNB, FMAS (Obstetrics and Gynecology)


Dr. Jain is a member of the AAGL Urogynecology and Vaginal Surgery SIG Board and Director in the Department of Obstetrics and Gynecology at Ganesh Shankar Vidyarthi Memorial (GSVM) Medical College at Kanpur University in Uttar Pradesh, India.
Dr. Sureddi is a member of the AAGL Urogynecology and Vaginal Surgery SIG and a Fellow in Gynae Endoscopy at Vardhman Trauma and Laparoscopy Centre in Uttar Pradesh, India.

The Case of the Dynamic Cyst
An 81-year-old G2P2 presented to an outside hospital Emergency Department (ED) with difficulty urinating and abdominal pain. She reported diminishing urinary output in the preceding 3-4 days, with only a small trickle upon standing on the day of presentation. She denied any previous bladder concerns. Her abdominal pain was severe, isolated to the lower abdomen and refractory to acetaminophen. She reported lower abdominal fullness. She denied any upper abdominal pain, nausea or emesis, issues with defecation, and her review of systems was otherwise unremarkable.
Her past medical history was notable for hyperlipidemia, hypertension and Sjogren’s syndrome. Her past surgical history was significant for a total abdominal hysterectomy in her 40’s for heavy menstrual bleeding and a laparoscopic cholecystectomy. She was a non-smoker, not sexually active, and historically had two uncomplicated vaginal deliveries. Her BMI was 32 kg/m2.
On her exam in the ED, she was noted to have a distended suprapubic region with tenderness to palpation. A CT scan showed a distended urinary bladder with bilateral hydronephrosis. She was also noted to have a 7.8cm cystic lesion or fluid collection posterior and inferior to the urinary bladder at the level of the vagina (Image 1). Her kidney function was normal, but her urinalysis was concerning for UTI, so she was started on a cephalosporin. Of note, no pelvic exam was performed.
 Image 1: Initial CT Scan
Image 1: Initial CT Scan
A foley catheter was placed in the ED which drained 1.2L of urine and she was transferred to our institution for further evaluation. A pelvic exam demonstrated a large, non-tender mass, approximately 7-8 cm in length along the anterior vaginal wall. Both Skene’s glands were visible and unremarkable. Fluid was attempted to be milked out the urethra, however no fluid was expressed. At this time her catheter remained in place for treatment of her distention injury.
The differential diagnosis at this time favored Gardner’s duct cyst, but urethral diverticulum, and Skene’s gland cyst were also considered. It was hypothesized the large cyst caused bladder outlet obstruction, resulting in her urinary retention and hydronephrosis.
She followed up in a urogynecology clinic for catheter removal and surgical planning. Her history was corroborated, and on exam, the cyst was noted to be much smaller in size, ~3 x 3cm in size. She passed a retrograded voiding trial, and her catheter was removed. An MRI revealed a loculated cystic collection measuring 2.8 x 2.2 x 3.6cm within the upper aspect of the vaginal canal with rim enhancement but no solid component (image 2). The read noted that although this was favored to relate to a Gartner’s duct cyst, given its interval decrease in size, the possibility of a urethral diverticulum was not excluded.
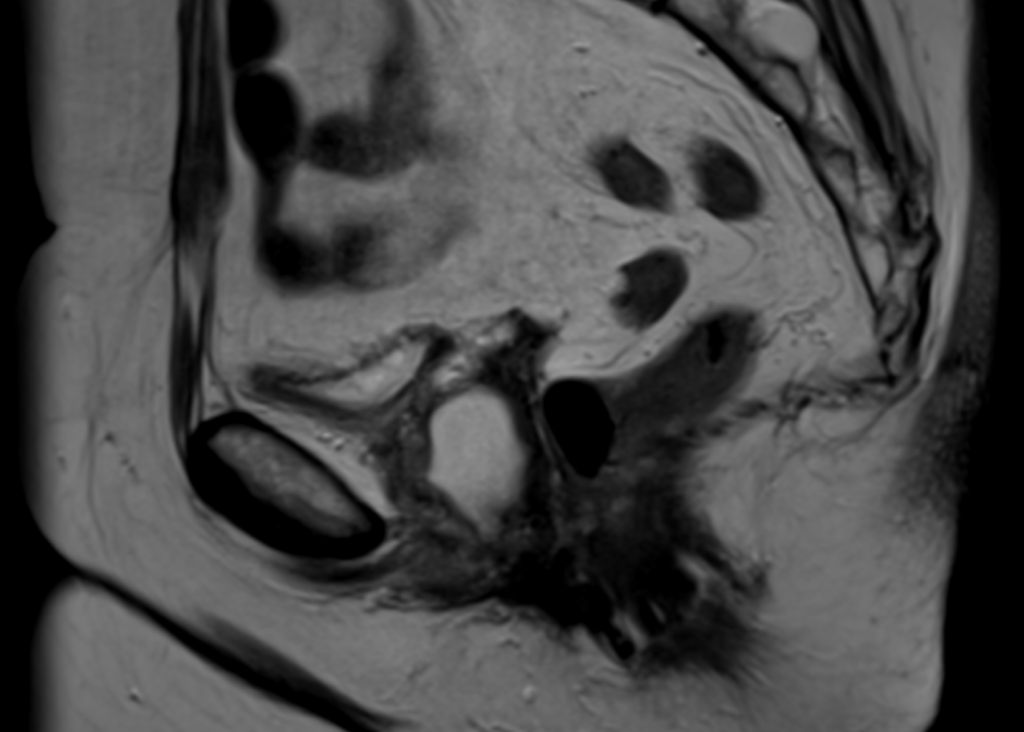 Image 2: Interval MRI
Image 2: Interval MRI
Given the discordance of her hospital and office exam, the decision was made to perform an exam under anesthesia and cystourethroscopy. On exam, she was noted to have a proximal anterior vaginal wall cyst from which fluid could be milked out of the urethral meatus with palpation. A cystoscopic survey of the bladder was unremarkable, however on urethroscopy a single large ostia was noted approximately 1 cm distal to the bladder neck, just to the left of midline (Image 3). A urothelial-lined diverticular sac was appreciated. The cyst became more distended by the cystoscopy fluid. She was diagnosed a urethral diverticulum and is scheduled to undergo a vaginal urethral diverticulectomy with possible martius flap.
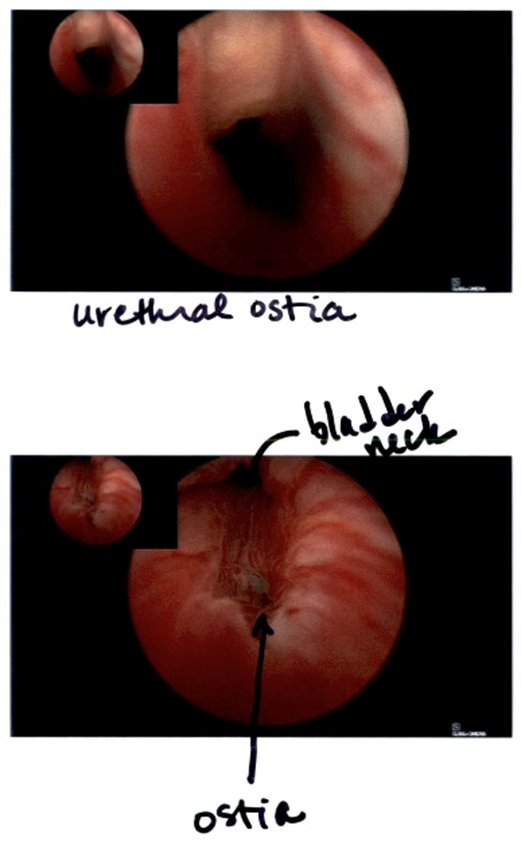 Image 3: Cystoscopy Finding
Image 3: Cystoscopy Finding
About the Author
Lisa Hickman, MD

Dr. Hickman is Vice-Chair of the AAGL Urogynecology and Vaginal Surgery SIG, Associate Professor in Urogynecology & Reconstructive Pelvic Surgery and Founder and Director of the Childbirth Pelvic Floor Disorders Clinic at Ohio State University Wexner Medical Center in Columbus, Ohio.
The post Spotlight On: Urogynecology and Vaginal Surgery appeared first on NewsScope.
