
This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Oncology Special Interest Group (SIG) led by Chair, Yukio Sonoda, MD.
Access to SurgeryU and JMIG are two of the many benefits included in AAGL membership. The SurgeryU library features high-definition surgical videos by experts from around the world. JMIG presents cutting-edge, peer-reviewed research, clinical opinions, and case report articles by the brightest minds in gynecologic surgery.
SurgeryU video recommendations by our SIGs are available for public access for a limited time. The links to JMIG article recommendations are accessible by AAGL members only. For full access to SurgeryU, JMIG, CME programming, and member-only discounts on meetings, join AAGL today!
NEW! SIG Recommended SurgeryU Video #1:
Minimally Invasive ICG Sentinel Lymphonodectomy in Vulvar Cancer in 10 Steps
Stefan Mohr, Sara Imboden, Franziska Siegenthaler, and Michael D. Mueller
This beautiful surgical video shows the technical details involved in Sentinel node harvesting aided by ICG /Fluorescence technology. This method provides excellent vision of both lymph vessels and lymph nodes, allowing minimal incisions thus reducing classical related wound morbidity.
SIG Recommended SurgeryU Video #2:
Benign Gynecologists’ Approach to the Adnexal Mass
Jubilee Brown
This superb Webinar discusses thoroughly all aspects related to adnexal masses when encountered by the general gynecologist. From initial workup to actual surgical tips, when to refer, “what to do if´s” and much more delivered by Dr. Brown in a relaxed and familiar way. Enjoy it!
JMIG Article Recommendation #1:
Jennifer Mateshaytis, MD, MSc, Pat Trudeau, RN, BN, Steven Bisch, MD, MPH, Sophia Pin, MD, MSc, Michael Chong, MD, Gregg Nelson, MD, PhD
This QI study demonstrated that the ERAS QI initiative resulted in a substantial increase in same day discharges (SDD) in patients undergoing minimally invasive Gyn Onc (GO) procedures. The investigators also showed that implementation of simple, clearly defined QI interventions to achieve higher rates of SDD, is feasible. This suggests that an ERAS SDD program for GO could be a realistic goal for centers aiming to attain higher rates of SDD in this patient population.
JMIG Article Recommendation #2:
Analysis of Sociodemographic Factors Affecting Ambulatory Surgical Center Discharge Patterns for Endometrial Cancer Hysterectomies
S. Wang, C. Moore, K. Das, C. Wu, N. Chappell
In this article, the authors explored the feasibility and discharge outcomes for minimally invasive hysterectomies (MIH) for endometrial cancer in ambulatory surgery centers (ASC). The authors demonstrated that MIHs for endometrial cancer are feasible in an ASC. However, the authors also identified patients who would be better suited to undergo MIH in this setting. Optimal candidates included patients who were younger, with less comorbidities, and lower body mass index.

Streamlining Sentinel Node Mapping in Vulvar Cancer
The management of early-stage vulvar cancer includes resection of the primary tumor with lymph node evaluation traditionally accomplished with a full inguinofemoral lymphadenectomy. However, the minority of patients with early-stage vulvar cancer have positive nodal disease. Consequently, many patients will undergo unnecessary lymphadenectomy with the associated surgical morbidity, i.e. chronic lymphedema (30-70%) and wound breakdown (20-40%).1 To mitigate such surgical morbidity, the sentinel lymph node (SLN) procedure was introduced to identify the most proximal draining lymph node from the tumor.
In the GROINSS V-I study, patients with negative SLN did not undergo inguinofemoral lymphadenectomy, and the groin recurrence rate in these patients was 2.5% (after 105 months of follow up).2 Lymphedema was reduced from 25.2% (n=30 of 144) in patients with positive SLN who underwent inguinofemoral lymphadenectomy to 1.9% (n=5 of 264) in patients who only had SLN biopsy.3 The GOG-173 study showed similar results with a false-negative predictive value of 2.0% (for tumors <4cm).4 Following these studies, the SLN procedure became the new standard of care for patients with early-stage vulvar cancer.
In these studies, SLN mapping was preformed using preoperative lymphoscintigraphy in conjunction with intraoperative blue dye visualization. Preoperative lymphoscintigraphy employs a radiocolloid injection and nuclear imaging. During surgery SLN identification is carried out using a nuclear probe and blue dye.
The use of radioactive tracers involves ionizing radiation, high costs, and time-consuming preoperative procedures.5 Blue dye can also obstruct the surgical field. Indocyanine green (ICG) offers an alternative to these tracers. ICG is a contrast agent visualized with near-infrared (NIR) fluorescent light (700 nm – 900 nm), which penetrates tissue more deeply (depth of detection is about 5 mm) compared to visual light.5 Because NIR is invisible to the human eye, ICG does not alter the surgical field, and there is no radiation exposure.5 Multiple studies have established the efficacy of NIR fluorescence with ICG for SLN biopsy in endometrial and cervical cancer, which is now the standard of care.
The ongoing Vulvar ICG SLN Detection (VISION) trial is designed to compare the efficacy of ICG with NIR fluorescence against standard radiocolloid lymphoscintigraphy for detecting SLN in early-stage vulvar cancer. Patients will undergo standard preoperative lymphoscintigraphy; however, the surgeon will be blinded to the results and initially ICG will be used to identify the SLN and remove it. After removal, the lymphoscintigraphy results will be revealed, and a gamma-ray probe will be used to confirm the SLN and evaluate the inguinofemoral lymph node bed for any more proximal nodes.
A retrospective review comparing SLN mapping modalities in vulvar cancer (e.g., TC-99 alone, blue dye alone, ICG alone, TC-99 + ICG, TC-99 + blue dye, TC-99 + blue dye + ICG, blue dye + ICG) demonstrated a detection rate of 96.2% regardless of technique used.9 The VISION trial will hopefully provide evidence supporting the use of NIR fluorescence with ICG alone as a viable replacement for lymphoscintigraphy to detect SLN in vulvar cancer.
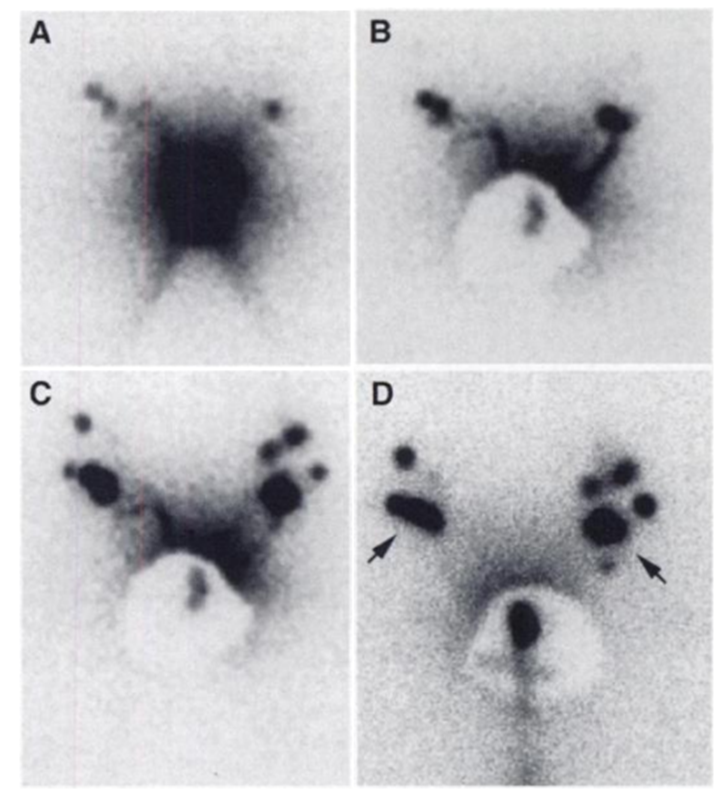
Figure 1. Lymphoscintigram of Patient 4 with a T2 tumor on the right side of the clitoris. Graphs were selected from a dynamic series. A and B were recorded 5 and 10 minutes after administration of tracer, without (A) and with (B) shielding of the primary tumor. On the right side of two sentinel nodes are shown and on the left side one sentinel node is shown. C and D were recorded 30 and 150 minutes after administration of tracer. Overflow to nonsentinel nodes is clearly visible on both sides. The arrows in D point to the nodes that were regarded as sentinel nodes.
https://www.nature.com/articles/6690918
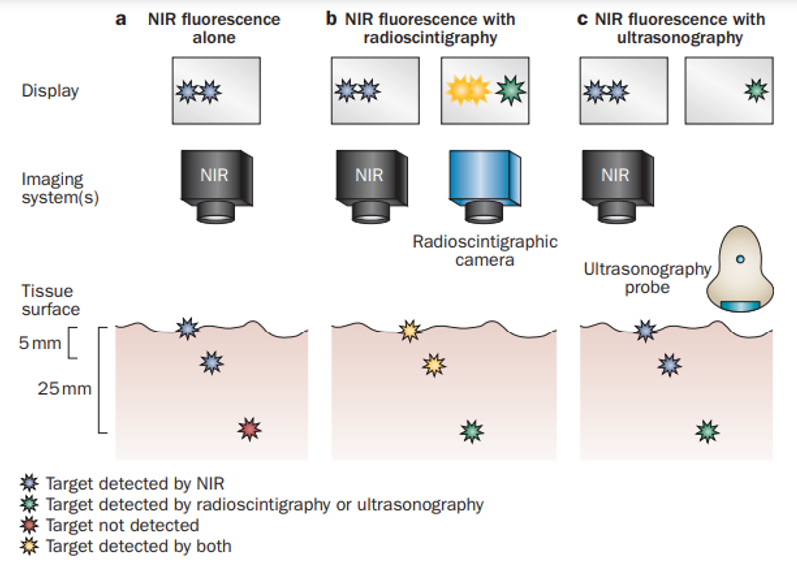
Figure 2. Near-infrared (NIR) fluorescence imaging alone or in combination with other imaging modalities. a. In this example, two superficially located targets (up to 5-8mm deep), can be located using NIR fluorescence imaging. However, a deeper target (at 25mm) would be invisible using by NIR fluorescence imaging alone. b. Combining NIR fluorescence imaging with radioscintigraphy enables visualization of all three targets. Once overlying tissue is surgically removed as guided by radioscintigraphy, NIR fluorescence can be used for more-precise image guidance. c. Intraoperative ultrasonography can visualize targets that are located deeper in tissue than NIR imaging but fails to find superficially located targets because of high acoustic reflectance. However, these superficial targets can be visualized by NIR fluorescence. Of note, the ultrasound prove must be in direct contact with the tissue being imaged, precluding simultaneous imaging with NIR fluorescence.
https://www.nature.com/articles/nrclinonc.2013.123
References
- Wagner MM, van der Zee AGJ, Oonk MHM. History and Updates of the GROINSS-V Studies. Cancers. 2022;14(8):1956. doi:10.3390/cancers14081956
- te Grootenhuis NC, van der Zee AGJ, van Doorn HC, et al. Sentinel nodes in vulvar cancer: Long-term follow-up of the GROningen INternational Study on Sentinel nodes in Vulvar cancer (GROINSS-V) I. Gynecol Oncol. 2016;140(1):8-14. doi:10.1016/j.ygyno.2015.09.077
- Van der Zee AGJ, Oonk MH, De Hullu JA, et al. Sentinel Node Dissection Is Safe in the Treatment of Early-Stage Vulvar Cancer. J Clin Oncol. 2008;26(6):884-889. doi:10.1200/JCO.2007.14.0566
- Levenback CF, Ali S, Coleman RL, et al. Lymphatic Mapping and Sentinel Lymph Node Biopsy in Women With Squamous Cell Carcinoma of the Vulva: A Gynecologic Oncology Group Study. J Clin Oncol. 2012;30(31):3786-3791. doi:10.1200/JCO.2011.41.2528
- Vahrmeijer AL, Hutteman M, van der Vorst JR, van de Velde CJH, Frangioni JV. Image-guided cancer surgery using near-infrared fluorescence. Nat Rev Clin Oncol. 2013;10(9):507-518. doi:10.1038/nrclinonc.2013.123
- Buda A, Crivellaro C, Elisei F, et al. Impact of Indocyanine Green for Sentinel Lymph Node Mapping in Early Stage Endometrial and Cervical Cancer: Comparison with Conventional Radiotracer 99mTc and/or Blue Dye. Ann Surg Oncol. 2016;23(7):2183-2191. doi:10.1245/s10434-015-5022-1
- Frumovitz M, Plante M, Lee PS, et al. Near-infrared fluorescence for detection of sentinel lymph nodes in women with cervical and uterine cancers (FILM): a randomised, phase 3, multicentre, non-inferiority trial. Lancet Oncol. 2018;19(10):1394-1403. doi:10.1016/S1470-2045(18)30448-0
- Papadia A, Gasparri ML, Buda A, Mueller MD. Sentinel lymph node mapping in endometrial cancer: comparison of fluorescence dye with traditional radiocolloid and blue. J Cancer Res Clin Oncol. 2017;143(10):2039-2048. doi:10.1007/s00432-017-2501-8
- Broach V, Abu-Rustum NR, Sonoda Y, et al. Evolution and outcomes of sentinel lymph node mapping in vulvar cancer. Int J Gynecol Cancer. 2020;30(3). doi:10.1136/ijgc-2019-000936
About the Authors
Katherine Foug
Yukio Sonoda, MD
Katherine Fong is an MD Candidate, Class of 2025, at the University of Michigan Medical School in Ann Arbor, Michigan.
Yukio Sonoda is Chair of the AAGL Oncology SIG and is attending Surgeon at Memorial Sloan Kettering Cancer Center in Manhattan, New York.
The post Spotlight On: Oncology appeared first on NewsScope.



